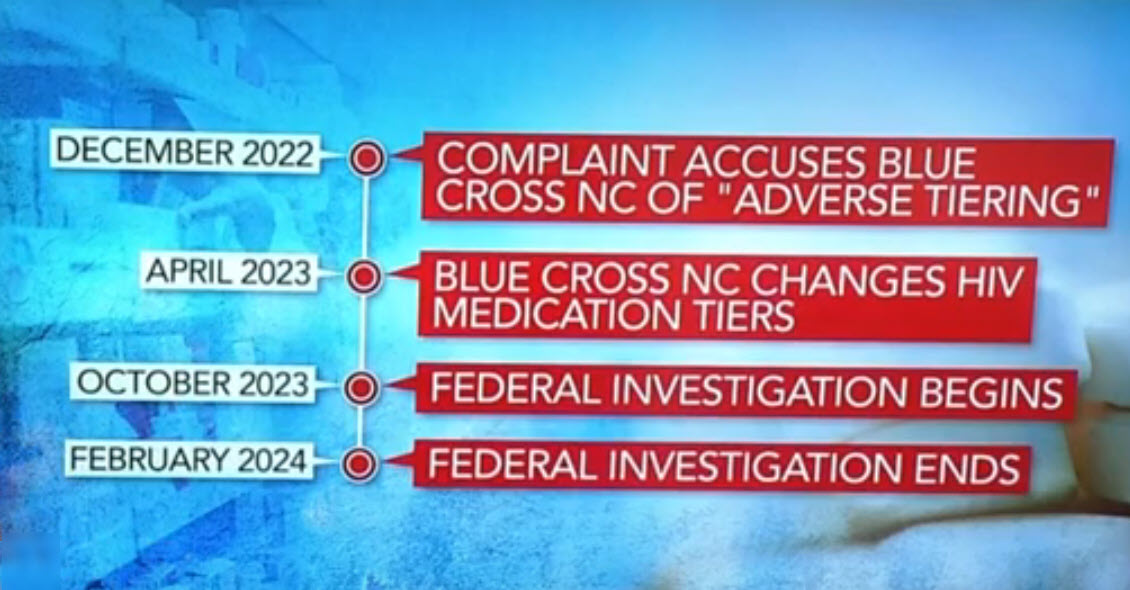
The federal investigation into Blue Cross and Blue Shield of North Carolina, the state’s largest health insurer, has officially come to an end. The U.S. Department of Health and Human Services concluded its examination of a complaint filed against the insurer over a year ago.
The investigation stemmed from allegations made by several advocacy groups, accusing Blue Cross of discriminatory pricing practices related to medications for patients with HIV. The complaint prompted a thorough review by the U.S. Department of Health and Human Services into the insurer’s pharmaceutical pricing policies.
According to sources, Blue Cross took corrective action following the filing of the complaint, specifically lowering out-of-pocket prices for HIV medications. This move was seen as a response to the concerns raised by advocacy groups and an effort to address the perceived discriminatory practices.
In a recent development, the U.S. Department of Health and Human Services opted not to issue any penalties against Blue Cross. The decision was based on the insurer’s corrective measures and the apparent resolution of the issues highlighted in the complaint.
The conclusion of the federal investigation marks a significant milestone for Blue Cross and Blue Shield of North Carolina. While the complaint initially raised questions about the insurer’s pricing strategies, the resolution signals a commitment to rectifying identified concerns and maintaining compliance with healthcare standards.
Blue Cross has not released an official statement regarding the investigation’s conclusion, but industry experts anticipate that the insurer will likely emphasize its dedication to providing equitable healthcare access to all its policyholders.
As the case formally closes, it brings attention to the ongoing scrutiny of healthcare practices, highlighting the role of advocacy groups in holding major insurers accountable for fair and unbiased policies.