A former employee of UnitedHealthcare, one of the nation’s largest health insurance providers, has come forward with allegations that the company systematically trained staff to deny claims. The whistleblower’s statements have ignited widespread concern over the practices of insurance companies and their impact on patients seeking essential healthcare services.
The ex-employee, who worked within UnitedHealthcare’s claims department, claims that staff were instructed to find ways to reject insurance claims, even when they appeared to be valid. According to the whistleblower, this practice involved emphasizing procedural loopholes, technicalities, and ambiguous policy language to deny coverage. The former employee alleges that denying claims was part of a broader strategy to minimize payouts and boost company profits.
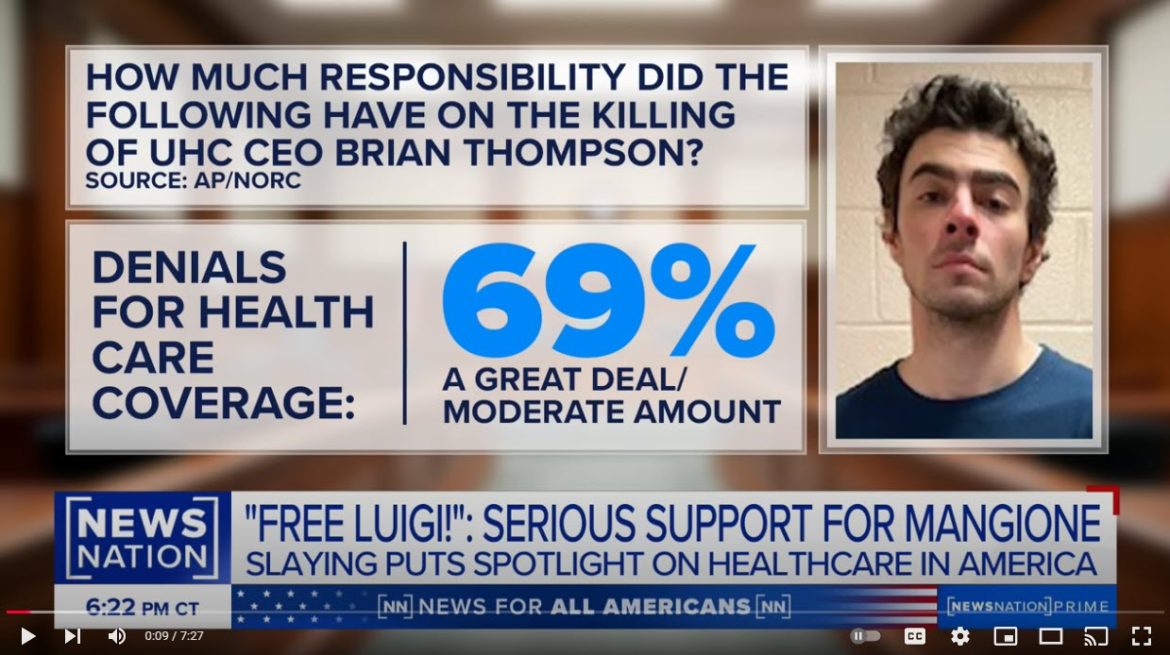
Patients impacted by denied claims often face significant challenges, including delays in receiving necessary medical treatments, financial hardship, and increased stress during critical health crises. The whistleblower’s allegations suggest that such denials were not isolated incidents but rather part of an institutionalized approach to reduce the company’s liability.
Healthcare advocates and consumer rights organizations have condemned the reported practices, calling for immediate investigations into UnitedHealthcare and other insurers suspected of similar behavior. They argue that such actions undermine the trust patients place in their health insurance providers and violate the ethical standards expected of companies in the healthcare industry.
UnitedHealthcare has not provided detailed comments on the allegations but has stated that it adheres to rigorous standards and reviews all claims fairly and transparently. The company asserts that claim denials are based on policy terms and medical necessity, and it maintains a process for appealing denied claims to ensure patients can seek redress.
Lawmakers and regulators are beginning to take notice of the growing controversy. Calls for hearings and stronger oversight of the health insurance industry have emerged, with officials emphasizing the importance of protecting consumers from unfair practices. Proposed reforms include greater transparency in claims processing, stricter enforcement of patient rights, and enhanced accountability for insurers.
The revelations come at a time when the U.S. healthcare system faces mounting scrutiny over rising costs, limited access to care, and the financial burdens placed on patients. Advocates are urging immediate action to address systemic issues and ensure that insurance providers prioritize the health and well-being of their policyholders over profits.
The former employee’s allegations highlight the complex dynamics of the health insurance industry and the critical need for reforms to safeguard patients. As investigations proceed, the focus remains on ensuring accountability and restoring trust in a system intended to provide security and support during medical emergencies.